In the latest installment of the GW Medicine Bicentennial Lecture Series, Julie E. Bauman, MD, led a panel of leading cancer researchers who explored the future of cancer treatment. The hour-long lecture, titled “Harnessing the Immune System Against Cancer — From Shots to Stem Cells,” delved into innovative therapies that empower the body’s natural immune system to fight cancer.
Bauman, who serves as the Dr. Cyrus Katzen Family Director of the George Washington University Cancer Center, associate dean of cancer at the GW School of Medicine and Health Sciences (SMHS), was joined by experts in the field, including Rong Li, PhD; Pavani Chalasani, MD; Amarendra Neppalli, MD; and Catherine Bollard, MD, representing GW’s work in gene regulation, engineered antibodies, stem cell transplantation, and adoptive cell therapy, respectively.
Highlighting the discussion was a powerful testimonial from cancer survivor Molly Cassidy, whose life was transformed by personalized immunotherapy treatment.
The Power of Immunotherapy: A Patient’s Story
Bauman first met Cassidy in 2018, after Cassidy had received treatment for stage 4 oral squamous cell carcinoma, a rare and aggressive form of head and neck cancer. At the time, Cassidy, an otherwise healthy 35-year-old, was a new mother, and on the brink of major life milestones — getting married, preparing to buy a house and studying for the bar exam.
“It was a very beautiful time in my life,” Cassidy recalled. “I should have been celebrating all of that beauty.”
Cassidy’s diagnosis was particularly grim: surgery to remove her tumor and surrounding tissue could impact her ability to speak, swallow and eat. She underwent an intensive treatment regimen that included oral surgery, removal of 34 lymph nodes, radiation and high-dose chemotherapy. Though physically and emotionally exhausting, Cassidy completed the grueling treatment and “rang the bell,” signaling her cancer’s remission.
The relief was short-lived. Not long after her remission, Cassidy discovered another tumor on her neck that spread rapidly throughout her mouth, her neck and then her lungs. At that point her options were limited.
Fortunately, she qualified for a groundbreaking clinical trial for a personalized immunotherapy vaccine. By analyzing her tumor’s genetic material, Bauman created a custom mRNA vaccine to target the specific mutations driving her cancer.
Preparing for the worst, Cassidy put her affairs in order and penned a stack of birthday cards and letters for each milestone she was likely going to miss in her son’s life; the first day at kindergarten, learning to drive, prom, high school and college graduation, getting married, even celebrating the birth of his own child.
Cassidy faced grueling regimen of vaccine infusion treatments, with regular CT Imaging to track her cancer. With each round of scans, however, her tumors grew smaller and smaller, then fewer and fewer, until one day there was no longer any evidence of her disease.
Four years later, she remains cancer-free.
“The research that you all are doing here gave me the gift of time … to live the beautiful life I had created,” she said to Bauman.
Cassidy’s life-saving therapy is just one aspect of the ongoing innovation at GW Cancer Center.
Going Beyond Barriers
Throughout the lecture, Bauman used an animated narrative to explain key elements of cancer research, framing the story around heroes and villains. The central “villain” is the tumor or cancer cell. The “superhero” is the T-cell, a type of white blood cell that leads the immune response by identifying and eliminating tumor cells. A third character, the “professor,” is the antigen-presenting immune cell, which teaches T-cells how to recognize and attack cancer cells. Bauman emphasized that each T-cell matches one specific “villain” or abnormal cell, and the interaction between the T-cell receptor and the tumor’s antigen is crucial for destroying the cancer.
However, cancer cells have evolved mechanisms to evade the immune system, making them successful in the body.
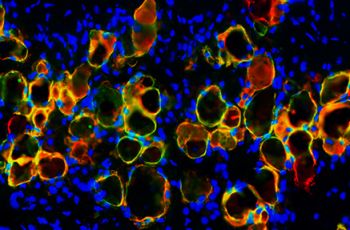
Rong Li, MD, chair of the Department of Biochemistry and Molecular Medicine and Ross Professor of Basic Science Research at SMHS, and a leading researcher in cancer and gene regulation, explained how tumor cells create an “immune shield” that prevents immune cells from attacking.
This shield, known as “immune exclusion,” is primarily made up of collagen fibers, which act as a physical barrier. Li’s team is working to understand the biochemical nature of this shield, how it forms and how to break it down. They discovered that a specific collagen receptor on the surface of tumor cells plays a key role in building the barrier.
By developing a neutralizing antibody that targets this receptor, Li’s team has been able to impair the shield in preclinical models, allowing immune cells to enter tumors and destroy cancer cells. This antibody is now undergoing phase I clinical trials for various solid-tumor cancers.
Immunotherapy and the Role of Antibodies
Next, Bauman shifted to the role of antibodies in cancer immunotherapy, focusing on how they can enhance T-cell activity against cancer cells.
Pavani Chalasani, MD, MPH, professor of medicine, and of biochemistry and molecular medicine, is the division director of hematology oncology. Chalasani also is a breast cancer medical oncologist with expertise in developmental therapeutics — turning laboratory discoveries into new medicines. She described the use of engineered antibodies as medicines to activate the immune system against cancer.
T-cells have both “activation” signals and “brakes” (such as PD-1 and PDL-1), which cancer cells exploit to suppress the immune response. Immunotherapy research has led to the development of antibody drugs that block the interaction between cancer cells and the T-cell brakes, specifically PD-1 and PDL-1 blockers.
If these blockers overstimulate T-cells, she warned, the immune system might attack healthy tissue leading to autoimmune disease. Monitoring for thyroid dysfunction is one way to manage these risks.
Looking ahead, Chalasani described new efforts to engineer antibodies, often referred to as drug antibodies, to deliver a chemotherapy payload directly to cancer cells like a “bio-missile.” The first such drug antibody was approved more than a decade ago. Today there are roughly 140 similar drugs in development, an indication of the promise of the approach.
An Early and Enduring Immunotherapy
For patients with blood-based cancer, such as leukemia or myeloma, the villains are literally flowing throughout their bodies. To treat these blood-based cancers, roughly 50 years ago researchers developed bone marrow transplantation. In the process, either autologous transplants (using the patient’s own stem cells) or allogeneic transplants (from a healthy donor), physicians collect the patient’s antibodies and safely store them before administering high-dose chemotherapy to kill cancer cells. After chemotherapy, the stem cells are returned to the patient to help restore their immune system.
Amarendra Neppalli, MD, associate professor of medicine, chief of Plasma Cell Disorders, and director of the Transplant and Cellular Therapy at GW Cancer Center, discussed classical approaches to stem cell transplantation, the earliest form of immunotherapy in cancer care.
The treatment process begins with checks to ensure the patient is fit for chemotherapy, including evaluating organ function and infection markers. The chemotherapy phase lasts two-three weeks, followed by a recovery period of an additional three-four weeks.
Recently, GW opened a state-of-the-art GMP Cellular Processing and Manufacturing Facility, a clinical requirement for the GW Cancer Center’s bone marrow transplant program. In addition to serving GW Cancer Center’s clinical care needs, the facility supports future clinical and translational cell therapy research, from clinical trials to the development of more novel therapies related to cell therapy.
Re-imagining the Immune Response
One of the most exciting developments in cancer treatment involves the extraction of naturally occurring T-cells in the body, re-engineering them and then reintroducing as an immunotherapy. Not every T-cell has the right receptor to match a cancer cell’s antigen, explained Bauman. To address this, scientists are working to reconfigure T-cells with the appropriate receptors, a process known as Chimeric Antigen Receptor (CAR) T-cell therapy.
Catherine Bollard, MBChB, MD, associate center director for translational research and innovation at the GW Cancer Center, is an internationally recognized clinician-scientist focused on adoptive cell therapy, when physicians take a patient’s own immune cells and alter them to become living medicines. Bollard, also a professor of pediatrics and director of the Center for Cancer and Immunology Research at Children’s National, explained that T-cells are the body’s primary defense against viral infections and cancer.
Bollard is working on CAR T-cell therapy targeting both solid tumors and liquid cancers, which involves attaching an artificial receptor to T-cells. The CAR T-cell can not only recognize tumors like an antibody, but also kill them like a T-cell. Originally developed for children with B-cell acute lymphoblastic leukemia, CAR T-cell therapy is now used to treat adult lymphoma and myeloma.
“In many cases,” she said, “we’re exploring strategies where CAR T-cells are used as a frontline therapy, even before considering a transplant. It has truly been a game-changer, especially for B-cell blood cancers.”
Another immune cell being re-engineered for cancer treatment is the “natural killer” (NK) cell. As the name suggests, NK cells are crucial in the immune system’s fight against invading cells. Unlike T-cells, NK cells aren’t patient specific and don’t trigger graft-versus-host disease when added to a patient. Bollard and her colleagues at GW are partnering with Children’s National to engineer NK cells with chimeric antigen receptors, creating an “off-the-shelf” treatment that could offer an alternative to the patient-specific approach used in CAR T-cell therapy.
A New Era of Cancer Care
Tying the lecture back to the broader vision of SMHS’s Bicentennial and the GW Cancer Center’s ongoing commitment to innovation, Bauman said, “We’re not just looking at the next great discovery; we’re working to ensure that these discoveries are accessible and transformative for all patients.”
As GW SMHS celebrates its 200th anniversary, she added, it’s clear that the next century of cancer research will be “defined by innovation such as personalized vaccines, re-engineered immune cells and cutting-edge treatments.”
“This is an era of cancer care that’s driven by the body’s own immune system — and the future has never looked more hopeful.”
Watch the video of the Bicentennial lecture, “Harnessing the Immune System Against Cancer — From Shots to Stem Cells” online.