The Division of Pulmonary, Critical Care, and Sleep Disorders Medicine at The George Washington University is proud to offer a three-year training program in pulmonary and critical care medicine in the heart of the nation’s capital. Twenty full-time pulmonary critical care or intensivists at the George Washington University Medical Center and the Washington DC VA Medical Center work to ensure a strong environment for clinical education and research.
Virtual Tour: Pulmonary and Critical Care Medicine
Thank you for your interest in our Pulmonary and Critical Care Medicine fellowship program. While we wish we could be meeting you in person, we are thrilled to offer you this virtual tour as an opportunity to see and learn more about the facilities and resources available to our fellows. Use the setting wheel icon in the top right corner to turn on the narration and the arrows at the bottom of the photos to see each stop. Click on the information buttons in the pictures to learn more about specific spaces and features. Click the gray icon in the top left corner for a full-screen view.
Directors
Current Fellows

Maxim Abu-Joudeh

Meher Alam

Benjamin DelPrete

Ahmad Hassan

Marwa Oudah

Lyndsey Turbow

Watipa Wendy Makhumalo
Education
The educational program is comprehensive. Below is a breakdown of the different components:
- Inpatient and Outpatient Care
-
Fellows gain experience in both inpatient and outpatient settings, which allows them to develop a broad understanding of the management of pulmonary conditions across different care settings.
- Pulmonary Radiology Sessions
-
These are dedicated sessions with radiologists who specialize in pulmonary imaging. Fellows can learn from these experts about the nuances of interpreting complex imaging findings related to the respiratory system. Additionally, fellows attend case review sessions involve reviewing and interpreting various types of imaging studies, specifically focusing on pulmonary-related conditions. This helps fellows enhance their skills in diagnosing and assessing pulmonary diseases through imaging.
- Multidisciplinary Tumor Board Conferences
-
Tumor board conferences involve a multidisciplinary team of healthcare professionals, including pulmonologists, oncologists, radiologists, and surgeons, who discuss and collaborate on the management of patients with lung cancer or other thoracic malignancies. Fellows can gain exposure to different perspectives and treatment approaches in this setting. Fellows are also encouraged to lead these conferences and discuss the cases that they have been following.
- Pulmonary Physiology Conferences
-
These conferences focus on understanding the physiological aspects of pulmonary function, such as lung mechanics, gas exchange, and respiratory physiology. Fellows can delve into the intricacies of how the respiratory system works and its relevance to clinical practice. With state-of-the-art Pulmonary Function Test Labs available in all our educational sites, fellows have the opportunity to attend PFT lab sessions in person and participate in performing various PFTs such as spirometry, lung volumes, and cardio-pulmonary exercise tests.
- Sleep-related Conferences
-
Sleep-related conferences are centered around the study and management of sleep disorders, such as sleep apnea, narcolepsy, and insomnia. Fellows can learn about the evaluation and treatment of these conditions, including the interpretation of sleep studies. In addition, fellows have the opportunity to attend the state-of-the-art sleep lab and participate in scoring and reading sleep studies.
- Critical Care Medicine Conferences
-
Critical care conferences would cover various aspects of managing critically ill patients, including medical, surgical, and neurosurgical critical illnesses. Fellows can enhance their knowledge and skills in the intensive care unit (ICU) setting and the management of patients with complex critical conditions.
- Journal Club-Research Conferences
-
Journal club sessions involve reviewing and discussing published research articles in the field of pulmonology and critical care medicine. This helps fellows stay updated with the latest advancements, learn critical appraisal skills, and develop an understanding of research methodology.
- Fellowship Bootcamp
-
The first-year fellows also attend a collaborative educational program at the start of fellowship designed by the faculties of various training programs in the DMV area. It is a four-week robust course that covers the basics of pulmonary and critical care medicine, specifically ventilator management. This provides them with a solid foundation for their subsequent training.
The Inpatient Experience

The inpatient training experience for pulmonary fellows is divided between two training sites, each offering unique experiences:
- The George Washington University Hospital
-
At this hospital, the pulmonary fellow takes the lead in managing an inpatient house staff team called the "Blue team." The team includes a resident, two interns and most of the time one or two medical students. The Blue team is responsible for caring for patients with primary pulmonary diagnoses, which may include conditions such as pneumonia, asthma or chronic obstructive pulmonary disease exacerbation, parenchymal lung diseases, pulmonary embolism, and other less common pulmonary conditions. The fellow also provides consultation services to other inpatients team, meaning they are called upon to offer their expertise in pulmonary medicine to help manage patients with respiratory issues.
During their inpatient rotation, fellows perform various procedures including bronchoscopy with bronchoalveolar lavage (BAL), endobronchial biopsies, endobronchial ultrasound-guided fine-needle aspiration (EBUS-FNA), robotic transbronchial biopsies, navigational bronchoscopy, radial EBUS, indwelling pleural catheter insertion, chest tube placement, and thoracentesis.
The GWU Hospital has a unique resource known as the Pulmonary Care Unit (PCU). The PCU is a specialized unit equipped with dedicated nursing staff, four patient beds, and continuous pulse oximetry and EKG monitoring. This unit allows for the initiation of non-invasive ventilation and the management of patients who require frequent nebulizer treatments or close monitoring. The pulmonary fellow at this site gains experience in managing patients with more complex respiratory conditions in a controlled and specialized setting.

- DC Veteran Affairs Medical Center (VA)
-
The pulmonary consult service at the VA medical center functions as a classic inpatient consultative service. Fellows on this service provide consultations for patients with pulmonary conditions admitted to the hospital and perform all procedures related to pulmonary medicine. The state-of-the-art bronchoscopy suite at the VA and our excellent faculty provide the opportunity to perform all pulmonary medicine related procedures. Fellows also have the opportunity to attend PFT labs at the VA center.
The Outpatient Clinic Experience
Overall, the inpatient training provides fellows with hands-on experience in managing a variety of pulmonary conditions, leading inpatient teams, and performing necessary procedures. The outpatient experience allows for longitudinal care and exposure to different patient populations, enhancing the fellows' clinical skills and breadth of knowledge in pulmonary medicine.
- DC Veteran Affairs Medical Center (VA)
-
First and second-year fellows typically have their continuity clinic at this center. They provide care for pulmonary outpatients under the supervision of attending staff. The clinics here also serve as a place to follow up with patients who have been discharged from the hospital, ensuring continuity of care.
- GW Medical Faculty Associates Clinic
-
All PGY-6 and occasionally one of the PGY-5 fellows will have their outpatient clinic at this location. Fellows have their own clinic supervised by an attending physician. The aim of this arrangement is to maximize continuity of care while also exposing fellows to a broader range of clinical conditions and patient populations.
The Critical Care Experience
The fellowship program is designed to provide each trainee with sufficient exposure to critical care medicine. This learning process includes acquiring the cognitive skills to evaluate and manage critically ill patients, as well as the development of procedural skills. The fellows rotate at two clinical sites; VA Medical Center and The George Washington University Hospital.
- Medical ICU
-
The Medical Intensive Care Unit at the VA Medical Center provides an opportunity for fellows to care for critically ill veterans. A wide variety of medical illnesses are encountered, and fellows work under the supervision of attending staff. This ICU is a purely medical ICU.
- GWU Hospital ICU
-
The Intensive Care Unit at the George Washington University Hospital is a large, multidisciplinary ICU located on four different floors. The hospital is a city-designated Level 1 trauma center located above the Foggy Bottom metro station. During the GW ICU rotation, pulmonary and critical care fellows are responsible for the management of patients with a variety of medical, surgical, or neurosurgical conditions. The fellows are encouraged to do all the ICU related procedures under the supervision of their attendings.
The GW University Hospital has an active cardiac catheterization lab and cardiothoracic surgery program, fellows also gain experience in the management of patients on intra-aortic balloon pulsation, extra-corporeal membrane oxygenation (ECMO), Impella and right ventricular assist devices (RVAD).
The training experience is enriched by close interaction with attending staff, other critical care fellows, and house staff, who together represent a variety of backgrounds including general surgery, anesthesiology, emergency medicine, neurosurgery, and internal medicine.
In addition to that, there is a special focus on POCUS and the critical care faculty arranges dedicated teaching sessions throughout the year to enhance POCUS skills of the fellows.
For more information, please visit the GWU ICU website.
Pulmonary Function Test Lab
All training sites have pulmonary function laboratories capable of doing spirometry, flow volume studies, lung volumes, diffusing capacity, arterial blood gas analysis and exercise studies. During the fellowship, fellows will learn how to perform and interpret PFTs. Fellows will also supervise inhalation challenge and exercise tests.
Fellows are expected to initiate clinical research protocols during their PFT/research rotation. During this rotation, trainees also have time to attend Sleep lab, participate in performing bronchoscopy or gain experience in endotracheal intubation with anesthesiologists.
The Lung Transplantation and Advanced Lung Disease Rotation
Early in their third year of fellowship and occasionally during their second year, fellows rotate through INOVA Fairfax Hospital’s Advanced Lung Disease and Transplant Program. Fellows from GW as well as other medical centers are involved in all aspects of care — evaluation of potential lung transplantation candidates, evaluation of potential lung donors, observation of lung transplant surgery and management of lung transplant recipients in the peri-operative period and in the outpatient setting. Experience is also gained in management of patients with pulmonary hypertension receiving continuous infusion of prostacyclin.
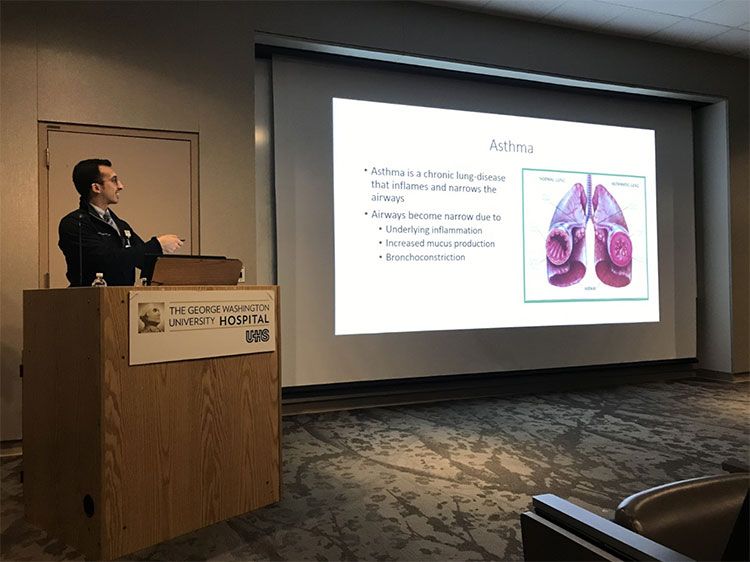
Academic Presentations
Fellows present at least two topics each year at the weekly core curriculum lecture series at GW. Typically, one of these topics is a pulmonary topic; the other is in critical care.
Fellows also take turns presenting interesting clinical cases at the quarterly meetings of the Metropolitan DC Thoracic Society, which is an official chapter of the American Thoracic Society. These meetings take place at the neighboring institutions including Howard University, Georgetown University, as well as at GW.
Additionally, academic presentations and journal clubs are given by the fellows rotating at the VA Medical Center.
Teaching Opportunities
Fellows are integral to our academic mission of training residents and educating students. While on the inpatient pulmonary service at GW, fellows lead the house staff team and are expected to actively teach the other members of the team. The intensive care units of both GW and the VA Medical Center represent prime opportunities to teach and discuss physiology and other aspects of patient management. The Division of Pulmonary, Critical Care, and Sleep Medicine has been honored to have our fellows repeatedly recognized as outstanding fellow of the year by the GW Internal Medicine House Staff.
Application Information
Applications are only accepted through the Electronic Residency Applications Service (ERAS).
The candidate must register for both ERAS and the National Residency Match Program (NRMP). A candidate who has not registered with the NRMP cannot be considered during the ranking process. It is very important to remember to register.
Requirements for GW Fellowships
Fellowship applicants must have completed three years in an ACGME-Accredited Internal Medicine Residency, and be board-certified or board-eligible.
Required Documents for Complete myERAS Application
- myERAS application
- Curriculum Vitae (CV)
- Personal Statement
- Three Letters of Recommendation (one from the program director)
- USMLE / COMLEX Scores (must have passed Steps I-III prior to start of fellowship year)
- Medical Student Performance Evaluation (MSPE)
- ECFMG Status Report for International Medical Graduates (must have certification)
- Licensing Information and Board-Eligibility/Certifications (if applicable)
- Citizenship Status
International Medical Graduates
We can only consider applicants with J1 visas. Please see our GME Visa policy.
IMGs must have completed an ACGME-accredited residency program.
Graduates of International Medical Schools must also be certified by the Educational Commission for Foreign Medical Graduates (ECFMG).
For more information, please visit the GW Graduate Medical Education website.
Research Experience
Direct involvement of every trainee in a research program enhances scholarly development, provides a foundation for logical and critical thinking, and encourages life-long habits of continuing scholarship. Through his or her research experience, each trainee will learn the design and interpretation of research studies, the evaluation of investigative methods, and the interpretation of data to develop competence in critical assessment of the medical literature. Fellows are given formal lectures on basic and functions of research.
During their first year, fellows are introduced to the research interest of the faculty. It is expected that during this year, each trainee will discuss projects with various faculty members and then decide on a research focus. One faculty member acts as a preceptor for the project and will meet frequently with the trainee to review his or her work. Research collaboration between multiple centers is strongly encouraged. It is fully expected that a trainee will initiate and complete one or two projects, including a quality improvement project (QI) during the fellowship training. Projects may include topics in pulmonary, critical care and sleep medicine. Fellows will have the opportunity to explore research ideas with basic sciences professor in the department of medicine. Throughout the years fellows have been involved in book chapter, review articles and clinical trials. Educational funding is available to permit each trainee to present an accepted paper or abstract at regional or national meetings.
Faculty
|
Jalil Ahari, MD |
Daniel Baram, MD Associate Professor of Medicine Director, Division of Pulmonary Medicine George Washington University Hospital |
|
Ivana Milojevic, MD |
Khalil Diab, MD |
|
Phue Khaing, MD |
Vivek Jain, MD |
|
Danielle Davison, MD |
Katrina Hawkins, MD |
|
Jeffrey Williams, MD |
Bruce Abell, MD |
|
Rahul Khosla, MD |
Kavita Vyas, MD |
|
Lawrence Lepler, MD |
Jeffrey Mikita, MD |
|
Svetolik Djurkovic, MD |
Lindsey Roschewski, MD |