“Prometheus was a titan who stole fire for the benefit of mankind,” said Armand Keating, M.D., FRCPC, director of the Cell Therapy Program at the Phillip S. Orsino Cell Therapy Translation Research Laboratory, professor of medicine at the Princess Margaret Cancer Centre and University Health Network, and professor at the University of Toronto’s Institute of Biomaterials and Biomedical Engineering. “This annoyed Zeus, so he bound Prometheus to a rock and had an eagle peck at his liver. The liver regenerated, and the eagle had to come back time and again to fulfill Zeus’s requirement.”
Keating’s storytelling came at the Dr. Leslie & Grazia Dornfeld and Lynda & Stewart Resnick Endowment’s Sixth Annual Great Teachers in Medicine Lecture, an annual event hosted by the Department of Medicine Grand Rounds and the GW School of Medicine and Health Sciences on April 30. Established in 2010 through the Dornfeld Trust, the endowed lecture honors and celebrates Dornfeld’s medical career and his passion for teaching the next generation of physicians.
“Why was Leslie known as such a good doctor?” asked Thor Stensrud, longtime Dornfeld family friend who spoke on their behalf at the event. “The answer that I’ve been able to come up with is he didn’t think there was any disease he could not diagnose. It was that perseverance and confidence, I think, that separated him from any of his peers.”
Now, the lecture brings renowned clinicians, like Keating, to GW to discuss innovative topics and trends in medicine. For Keating, innovation is clear in the classic Greek tale; Prometheus typifies what is becoming “a burgeoning” field: regenerative medicine.
“It’s a rapidly evolving, multi-disciplinary field that aims to replace, repair, and restore normal organ function or tissue by delivering safe, effective living cells either alone or in combination with specially designed materials,” Keating explained, referring to Professor Dame Julia Polak, renowned stem cell therapy researcher, and her description. “One thing we might add to Dame Julia’s definition is the use of soluble molecules, genetic engineering, tissue engineering, and advanced cell therapy.”
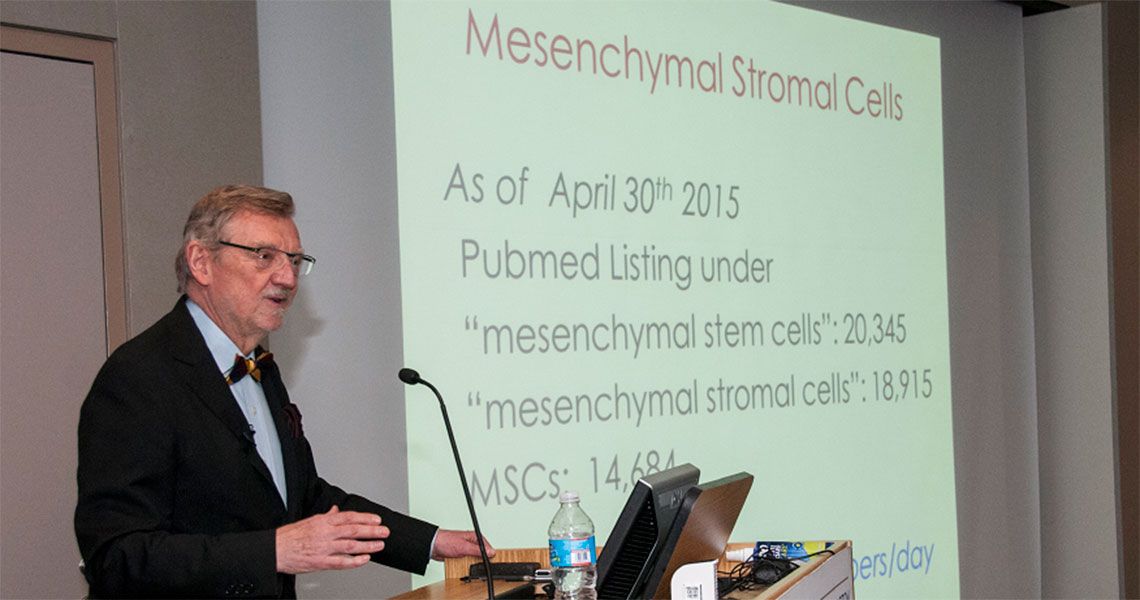
With those additions has come the rise of mesenchymal stromal cells (MSCs), which Keating asserts are different from the often-referred to stem cells.
“A stem cell is a cell that can undergo asymmetric division that gives rise to a daughter cell that remains a stem cell and another cell that becomes differentiated,” Keating said. “Because this is a really important point and it’s an issue that has been taken up by the press about stem cell therapy, I want to emphasize the limitations of that terminology. What we’re trying to do is to assess whether or not the cell population is capable of self-renewal and differentiation.”
With that ambiguity in terminology in mind, Keating focused on MSCs during a recent experiment. Using umbilical cord cells – perivascular cells with characteristics similar to those of bone marrow mesenchymal cells – Keating assessed whether they contributed to regeneration in a femur injury.
“The results are really quite revealing,” Keating said. “We studied the ability of those cells to undergo self-renewal and differentiation, and what we found was that, yes, indeed, there are stem cells present, but the frequency is extremely low: it’s one in 1,000. So, the population of cells that we’re dealing with is not really, truly a stem cell population any more than blood cells would represent them. Additionally, there’s no direct relationship between the tissue regeneration and those stem cell properties. That’s why I’ve called them mesenchymal stromal cells rather than stem cells. We can call them stem cells if we’re specifically referring to a stem cell population.”
Keating’s study on MSCs and cell therapy is just one of many, he said; between five and 10 new papers on regenerative medicine are published every day, and studies continue to determine how and why MSCs can be used for the treatment of so many disorders.
Keating offered one answer: “Human MSCs inhibit pro-inflammatory TH1 responses and increase TH2 anti-inflammatory responses. So that, I think, gives us a clue why MSCs are being considered as potential treatment for so many different diseases because they have an immune component, an inflammatory component, and so on.”
The future of MSCs is still cloudy, Keating said, as few researchers have offered long-term follow-up studies and there are several questions still to be answered: “Have we chosen the potent source [for cells]? Do we really understand the mechanism of action of these? Can we enhance their activity? Have we chosen the most appropriate indications based on our understanding of the mechanism? Did we design the trials in the best way?”
The first step toward the future, however, is clear.
“It’s time that we went back and really nailed the mechanisms of action,” Keating said. “Once we understand that, then I think we can design the most appropriate clinical trials. We’ll know the indications, we’ll know how to design those clinical trials, and Prometheus would be unbound if we succeed.”